Health - Flu & Infection Prevention - Banner

FLU & INFECTION PREVENTION
Health - Flu & Infection Prevention - Content
Flu prevention is in the air!
Can your air help prevent the spread of flu in your facility?
As has been shown in infection control reports, nine viruses have been identified as potential causes of respiratory diseases: Influenza virus, human coronavirus, human respiratory syncytial virus, Adenovirus, human bocavirus, Parainfluenza virus, human metapneumovirus, rhinovirus and enterovirus.
The majority of these viruses have pronounced seasonal outbreaks and the seasonal patterns of Influenza, human coronavirus and human respiratory syncytial virus evidently suggest a strong correlation with climatic factors.
The spreading of the above-mentioned viruses is primarily due to droplets from someone who is coughing, sneezing or even talking. Some reports even state that viruses could be airborne-transmissible through particles suspended in the air.
It all revolves around relative humidity. Why?
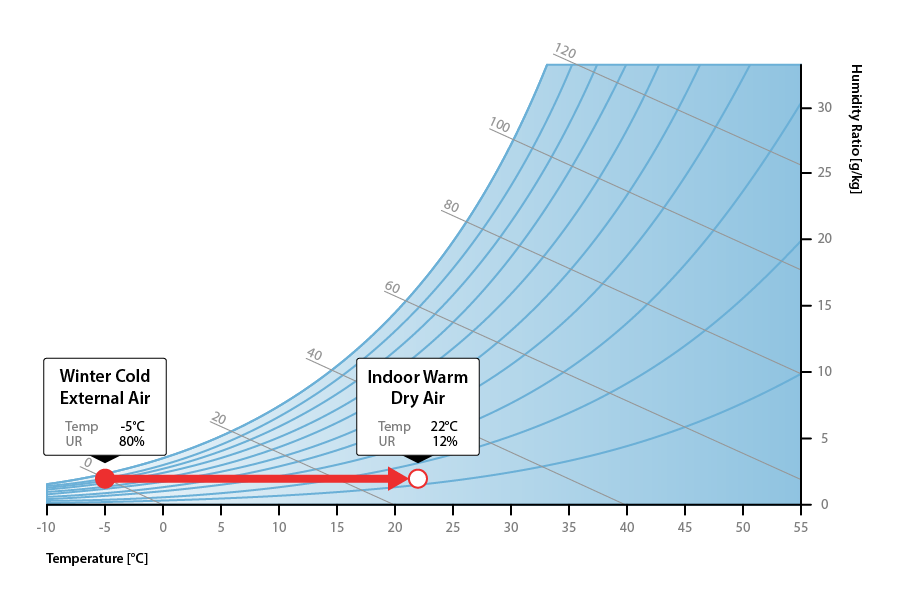
In winter, cold outside air means lower absolute humidity, which in turn leads to low relative humidity inside buildings, very often lower than 20%RH.
Human beings have not been "designed" for low humidity environments; indeed, a solid correlation has now been recognised between dry air and immune system impairment.
The effect of humidity on the viability of viruses
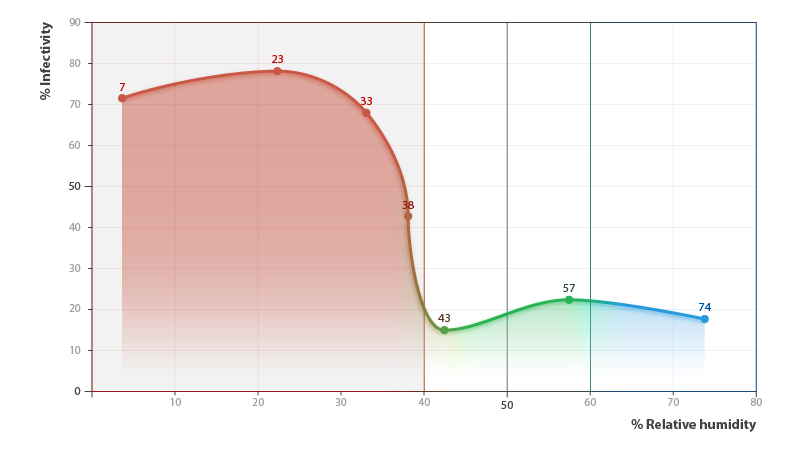
Lipid-containing viruses prefer low relative humidity (lower than 30%), whereas high relative humidity tends to favour the survival of viruses composed entirely of nucleic acids and proteins.
Several laboratory studies have examined the relationship between relative humidity and influenza virus survival or infectivity, and have shown that viral inactivation rates increase sharply at relative humidity above 40%.
The effect of humidity on our natural defences
Mucociliary clearance, or the mucociliary escalator, describes the self-clearing mechanism of the airways in the respiratory system. It is one of the two protective processes for the lungs in removing inhaled particles, including pathogens, before they can reach the delicate tissue of the lungs. The other clearance mechanism is the cough reflex. Mucociliary clearance has a major role in pulmonary hygiene.
Mucociliary clearance effectiveness relies on the correct properties of the airway surface liquid produced, both of the periciliary sol layer and the overlying mucus gel layer, and of the number and quality of the cilia present in the lining of the airways. An important factor is the rate of mucin secretion and thus the necessary hydration of the airway surface liquid.
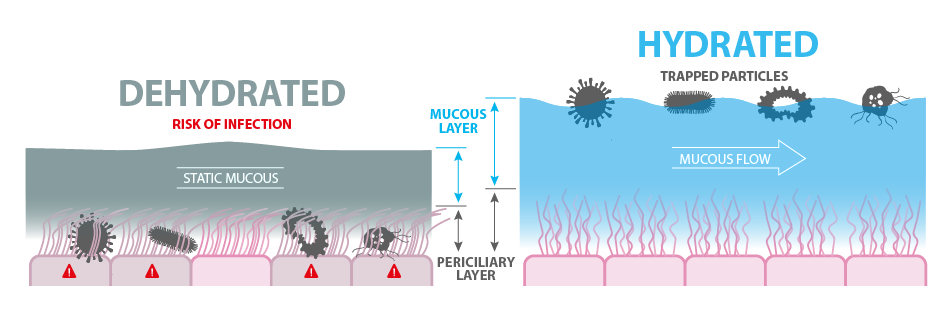
Analysis of the mucous in the trachea has shown that infection in low humidity conditions resulted in the inability of the cilia on the epithelial cells to move it. Low humidity in fact increased mucous thickness.
Infection at lower humidity compromises mucous clearance and impairs the immune system.
Health - Flu & Infection Prevention - Content 2
Air relative humidity control benefits
One of the best tools for fighting the spread of the flu in healthcare facilities is largely overlooked and underutilised. It lies in the air and the moisture content of that air. Relative humidity has a significant impact on infection prevention and transfer of the virus.
In 2013, NIOSH conducted a study looking at the infectivity of the flu virus at different RH% levels. It was found that once the RH% levels reached 40% and higher, there was a dramatic decline in the infectivity of the virus. It was found to be 85% ineffective once RH reached 43%. Added to the knowledge that higher RH% levels mean less travel time for any particles, keeping the proper levels of humidity during flu season can offer great benefits to patients and staff.
Mid-range air humidity between 40 and 60%, enhancing human immune system reaction, significantly reduces infections from seasonal respiratory viruses, saving thousands of lives threatened by seasonal respiratory illnesses.
Another positive social impact contribution of a proper air relative humidity control is on global health services. In fact, lowering healthcare-acquired infections means better service delivered to patients and at the same time improves both readmission rates and length of stays.

